Hepatitis C (HCV) is a virus that causes inflammation of the liver. Hepatitis means inflammation of the liver. It is a member of the family of viruses that include hepatitis A and hepatitis B. The viruses behave differently and have different modes of transmission. Hepatitis C can cause serious liver damage, liver failure, liver cancer, and even death.
 About 2.7-3.9 million people in the U.S. currently live with chronic hepatitis C infection.
About 2.7-3.9 million people in the U.S. currently live with chronic hepatitis C infection.
The World Health Organisation (WHO) has found that Egypt has the highest prevalence of the Hepatitis C virus (HCV) in the world, with approximately 22 percent of Egyptian blood donors testing positive for the deadly disease. It is estimated that roughly 15 million Egyptians currently suffer from Hepatitis C. Every year there are 170,000 to 200,000 new HCV cases.
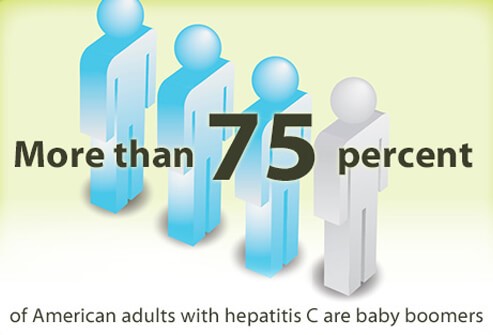
75%-85% of people infected with hepatitis C are infected with chronic hepatitis C. The virus is most common in baby boomers who represent 75% of infected adults. The rates of hepatitis C were the highest in the 1970s and 1980s, the time when many baby boomers were likely infected. Many people who have hepatitis C don't know they have it because the virus may not produce symptoms until decades after infection.
Hepatitis C in Children
Hepatitis C is less common in children, but there are approximately 23,000-46,000 children in the U.S. with hepatitis C. Most children are infected by hepatitis C at birth. A child has a 1 in 20 chance of being infected if the mother has hepatitis C. Adolescents can be infected with hepatitis C by exposing themselves to IV drug use, sharing needles, and high-risk sexual behaviors. Up to 40% of hepatitis C cases in children will go away on their own by age 2, if the virus is transmitted at birth.
 Hepatitis C is a blood-borne illness, meaning it is transmitted via contact with infected blood. Usually the virus enters the body through a puncture wound on the skin.
Hepatitis C is a blood-borne illness, meaning it is transmitted via contact with infected blood. Usually the virus enters the body through a puncture wound on the skin.
Is Hepatitis C Contagious?
Yes, hepatitis C is contagious. The most common way hepatitis C is transmitted is via injection drug use. Sharing needles with someone who is infected can transmit hepatitis C. Health care professionals may contract the virus via needlestick injury. Prior to 1992, the U.S. blood supply was not screened the way it is today, so some people contracted hepatitis C from infected blood transfusions. Rarely, babies born to hepatitis C-infected mothers acquire the virus. Hepatitis C can also be spread by having sex with an infected person or sharing personal items (a razor or toothbrush) with someone who has the virus, but these cases are rare.
 About 70% to 80% of people with the hepatitis C virus do not have any symptoms, especially in the early stages. In these people, symptoms may develop years, even decades later, when liver damage occurs. Others develop symptoms between 2 weeks to 6 months after infection. The average time to develop symptoms is 6 to 7 weeks after acquiring the virus. A person who has hepatitis C infection, but isn't exhibiting any symptoms can still pass the virus on to others. Hepatitis C symptoms may include:
About 70% to 80% of people with the hepatitis C virus do not have any symptoms, especially in the early stages. In these people, symptoms may develop years, even decades later, when liver damage occurs. Others develop symptoms between 2 weeks to 6 months after infection. The average time to develop symptoms is 6 to 7 weeks after acquiring the virus. A person who has hepatitis C infection, but isn't exhibiting any symptoms can still pass the virus on to others. Hepatitis C symptoms may include:

Acute hepatitis C infection refers to symptoms that appear within 6 months of newly acquiring the virus. About 20% to 30% of those who acquire hepatitis C experience acute illness. After this, the body either clears the virus or goes on to develop chronic infection.
Chronic hepatitis C infection refers to long-lasting infection. The majority of people who have acute hepatitis C infection (75% to 85%) go on to develop the chronic form of the illness.

Hepatitis C infection is diagnosed with several blood tests. The hepatitis C antibody test checks for antibodies (immune particles) that fight the virus. A "non-reactive" result means that antibodies to the virus are not detected. A "reactive" result means antibodies to the virus are present, but the test is unable to indicate whether the infection is current or from the past. Another blood test to assess the presence of hepatitis C genetic material (HCV RNA test) is available. The results of this test can help doctors determine whether hepatitis C infection is current or not. Additional blood tests can be used to determine the amount of virus in the body, known as a titer.
When someone has confirmed hepatitis C infection, the doctor will order more tests to assess the degree of liver damage. A liver biopsy may be performed. There are several different strains of the hepatitis C virus that respond to different treatments. For this reason, the doctor will order a test to determine the genotype(s) of the hepatitis C infection to help determine the course of treatment.
Who Should Get Tested for Hepatitis C?

Chronic hepatitis C infection is a long-lasting illness with potentially serious complications. About 75% to 85% of those with acute hepatitis C infection go on to develop chronic hepatitis C. Of those in the chronic illness group, more than two-thirds will develop liver disease. Up to 20% will develop cirrhosis, or scarring of the liver, within 20 to 30 years. Cirrhosis affects liver function and causes elevated blood liver enzymes. Up to 5% of people with chronic hepatitis C infection will die from liver cancer or cirrhosis. Chronic hepatitis C infection is the most common reason for liver transplantation in the U.S.
 Treatment for hepatitis C is available. The course of treatment depends on whether the infection is acute or chronic, the strain (genotype) of the virus, the amount of the virus in the body (viral load), the degree of liver damage, response to previous treatment, and the health of the patient. Hepatitis C treatment is highly individualized, so it's important to be under the care of a doctor with expertise in this area. The goal of treatment is to achieve sustained virologic response (SVR), which means there is no detectable virus in the blood 6 months after treatment. While it's not a cure, achieving SVR is the next best thing. Many people with hepatitis C can achieve SVR with treatment.
Treatment for hepatitis C is available. The course of treatment depends on whether the infection is acute or chronic, the strain (genotype) of the virus, the amount of the virus in the body (viral load), the degree of liver damage, response to previous treatment, and the health of the patient. Hepatitis C treatment is highly individualized, so it's important to be under the care of a doctor with expertise in this area. The goal of treatment is to achieve sustained virologic response (SVR), which means there is no detectable virus in the blood 6 months after treatment. While it's not a cure, achieving SVR is the next best thing. Many people with hepatitis C can achieve SVR with treatment.
Medications That treat Hepatitis C
Your doctor can choose the best treatment for your individual circumstances.
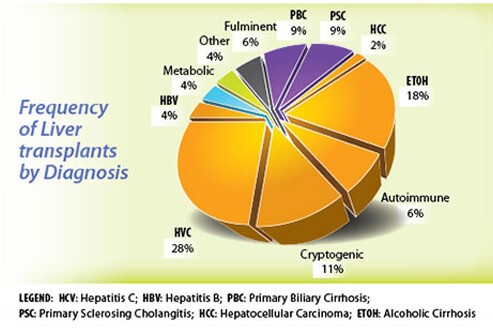
Some people with advanced hepatitis C and severe liver damage undergo a liver transplant, but that doesn't eradicate the infection. Patients with an active infection at the time of the transplant will develop hepatitis C in the new liver. Sometimes the infection recurs even when patients are on antiviral treatment. Those who have achieved sustained virologic response (SVR) - meaning no detectable virus in the blood 6 months after treatment - have a very low risk of developing hepatitis C infection in the new liver.

About 15% to 25% of people who are infected with the hepatitis C infection clear the virus on their own. Scientists are still trying to determine why hepatitis C goes away in some patients, while others go on to develop symptoms. There is no cure for an active or chronic hepatitis C infection, but sustained virologic response (SVR) is the next best thing. Hepatitis C infection rarely recurs in those who have achieved SVR.

There is currently no vaccine for hepatitis C. Research is ongoing to develop a vaccine against the virus. There are vaccines for hepatitis A and hepatitis B.
 Hepatitis C is a blood-borne infection. To reduce the risk of infection, avoid sharing personal items (toothbrushes and razors) with others. Do not use injected drugs. If you do use injected drugs, never share needles and equipment with others. Getting tattoos and body piercings can put you at risk. Use condoms during sex. Health care workers should take precautions to avoid needle-sticks and properly dispose of needles and other materials that come into contact with blood. Speak to your doctor about your risk factors and follow recommended screening standards for hepatitis C.
Hepatitis C is a blood-borne infection. To reduce the risk of infection, avoid sharing personal items (toothbrushes and razors) with others. Do not use injected drugs. If you do use injected drugs, never share needles and equipment with others. Getting tattoos and body piercings can put you at risk. Use condoms during sex. Health care workers should take precautions to avoid needle-sticks and properly dispose of needles and other materials that come into contact with blood. Speak to your doctor about your risk factors and follow recommended screening standards for hepatitis C.
How to Prevent Giving Hepatitis C
If you have hepatitis C, these common precautions should be followed to prevent spreading or giving hepatitis C to others: